Clinical applications
Plastic surgery / burn medicine
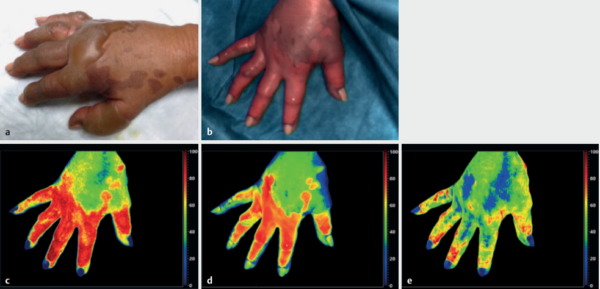
In plastic surgery, HSI technology is used, among other things, for the dynamic and pathophysiological assessment of flap plastics, grafts, and burn wounds. Poorly perfused flap plastics are not necessarily clinically noticeable visually for up to 72 hours after surgery. However, by the time poor perfusion can be detected, the skin flaps are already in poorer condition, thus more difficult to save, and cause greater revision effort.
With the TIVITA® Tissue it is possible for the doctor to identify oxygenation and perfusion problems in skin flaps, such as arterial insufficiencies and venous congestion, at an early stage and to initiate immediate corrective measures. This can reduce complications and significantly improve treatment outcomes after plastic reconstructive surgery.
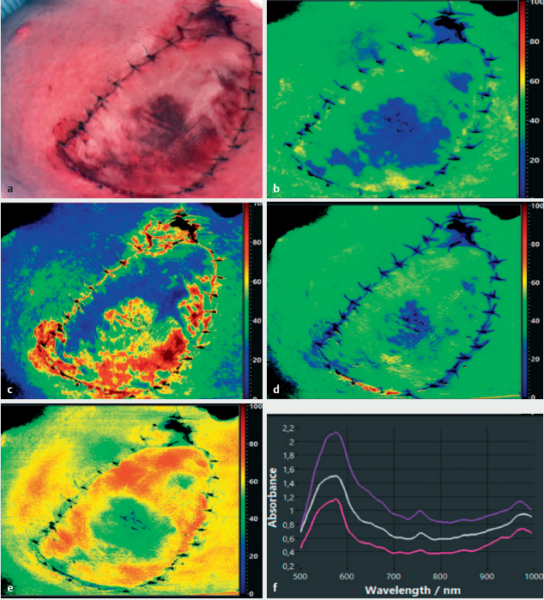
Furthermore, HSI technology provides a useful tool for objective assessment and evaluation of burns and their healing processes as well as for early prognosis of burn depth.