Klinische Anwendungen
Anästhesie und Intensivmedizin
Besonders bei kritisch kranken Patienten sind mikrozirkulatorische Veränderungen mit einer erhöhten Mortalität und Morbidität verbunden. Daher ist es in der Intensiv- und Notfallmedizin besonders wichtig, neben der Makrozirkulation, auch die Gewebeperfusion und Ödembildung zu monitoren, um die negativen Auswirkungen einer hämodynamischen Inkohärenz zu reduzieren.
Hier stellt das Hyperspektral-Imaging eine vielversprechende Methode dar, um bettseitig Veränderungen der Mikrozirkulation, Oxygenierung und des Wassergehalts der Haut zu monitoren. Probleme wie Medikamentendosisfehler, Kreislaufstörungen, pulmonale Komplikationen oder ineffiziente Sauerstofftherapien könnten somit frühzeitig erkannt werden. Der Gewebe-Wasser-Index, als Parameter eines Gewebe- oder Darmödems, kann z. B. indirekte Rückschlüsse auf die anästhesiologische Steuerung der intraoperativen Volumentherapie zulassen.
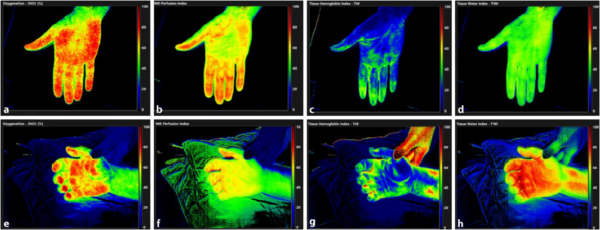
Dieses Beispiel zeigt sehr eindrucksvoll, die Fähigkeit der hyperspektralen Bildgebung mikrozirkulatorische/ödematöse Veränderungen in kritisch kranken Patienten bettseitig nachzuweisen. Somit kann frühzeitig die Therapie angepasst werden.